Recently, Prof. Zhang Yan of National Clinical Research Center for Geriatrics of West China Hospital, Sichuan University, Prof. Chen Lu of West China Second Hospital, and Prof. Wang Yuan of State Key Laboratory of Biotherapy, co-published a research paper titled "Sequential Fate-switches in Stem-like Cells Drive the Tumorigenic Trajectory from Human Neural Stem Cells to Malignant Glioma" online in Cell Research (IF: 20.5), a top international journal. The article analyzed the mechanism of malignant brain tumor in the elderly and the time window of early intervention.

As a primary brain tumor of the highest morbidity and mortality that mainly occurs among the elderly over 50 years old, Glioblastoma (GBM) has high heterogeneity and resistance to radiotherapy and chemotherapy, and the median survival period after treatment is only 15 months. An important reason for the poor prognosis of GBM is the lack of effective early diagnosis and intervention.
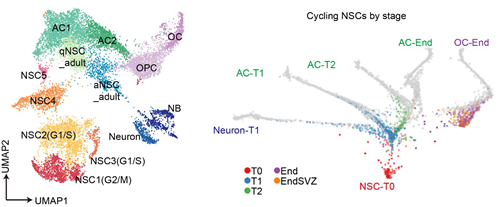
In this study, the authors successfully constructed a series of new malignant glioma models derived from human neural stem cells by knocking out GBM-related tumor suppressor genes TP53, NF1 and PTEN in human neural stem cells through gene editing, with a malignant tumor formation rate of more than 94%, simulating GBM of patients at pathological and molecular levels. Through multi-omics time series analysis, the panoramic map of malignant transformation of human neural stem cells into tumors in vivo was revealed for the first time at multiple time points, multiple levels and the single cell accuracy. The mechanism of dynamic transcription regulation at specific time points was established, and new tumor-promoting factors such as C1QL1 were discovered and verified. Through the construction of tumorigenesis trees and the pedigree tracking experiment, a kind of stem cell-like cell existing persistently in the tumorigenesis was found, which underwent many fate changes in the tumorigenesis and produced different malignant pedigrees in time and proper order. Short-term targeted intervention in these cells at early critical time points can effectively inhibit tumor occurrence, proving the time window for early diagnosis and treatment.
In general, this study established a new and efficient modeling method, and based on this, it showed the malignant transformation path from human neural stem cells to GBM in an overall perspective, demonstrating the importance for understanding the pathogenesis and heterogeneity formation of GBM and developing clinical early diagnosis and treatment strategies on this basis.
West China Hospital of Sichuan University is the first and corresponding author institute of the paper. Wang Xiaofei and Zhou Ran, PhD students in State Key Laboratory of Biotherapy, are the co-first authors.
Link to original text: https://www.nature.com/articles/s41422-020-00451-z
